Female Pelvic Floor and Common Dysfunctions
What is the Female Pelvic Floor
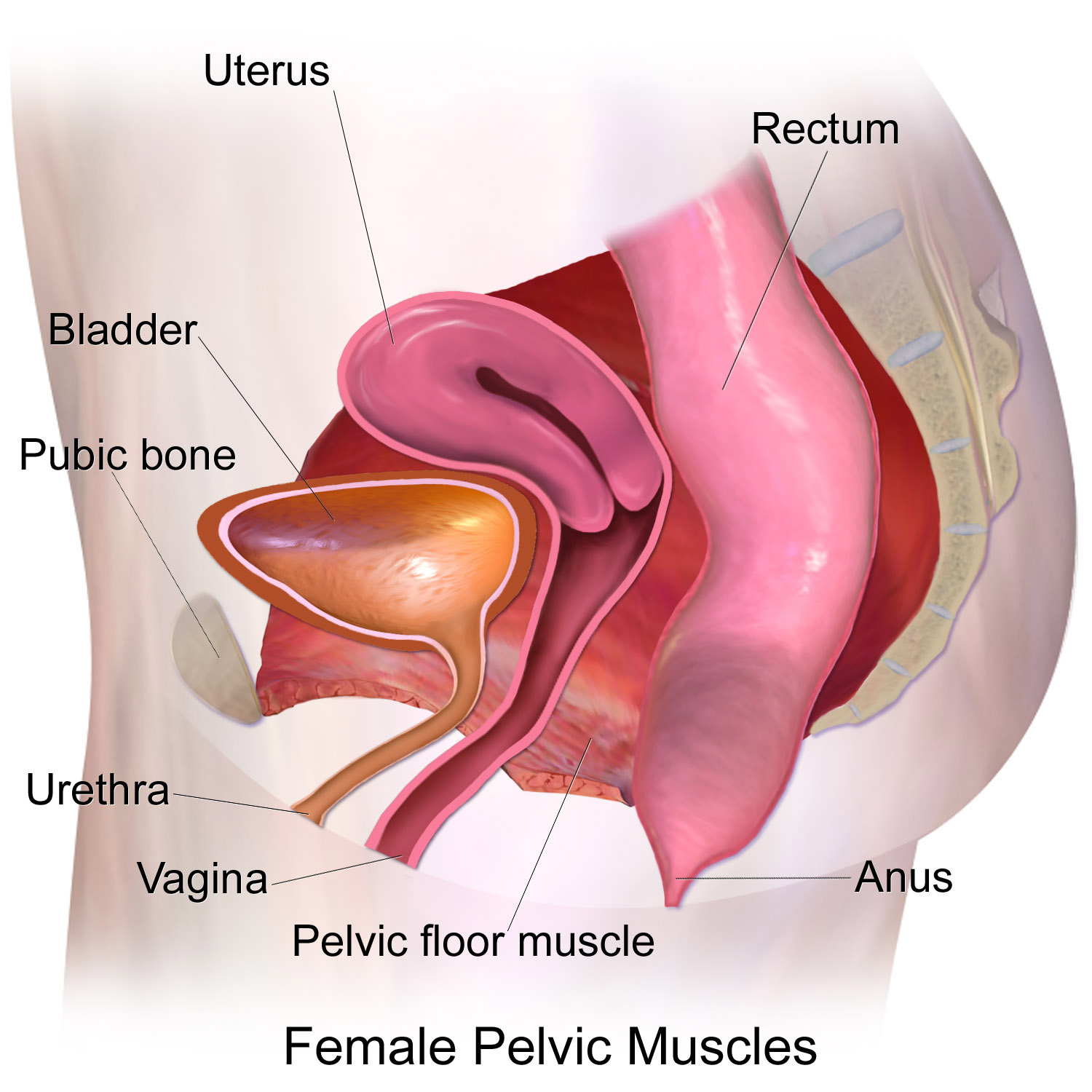
Pelvic Floor is a muscular hammock that lies across your vagina and anus that supports your bladder, uterus, vagina, rectum, and small bowel. These muscles can weaken or have disorders following childbirth, menopause, or any time in a woman's life. The purpose of the pelvic floor is to maintain urinary and bowel control and perform sexual function including orgasms.
Common Pelvic Floor Dysfunctions
A pelvic floor dysfunction (or disorder) is any condition whereby the pelvic floor no longer functions as it is meant to. By the age of 50, 50% of women experience one or more pelvic dysfunctions. These most commonly includes:
Urinary Incontinence – Involuntary urinary leakage from stress or pressure, or a sudden, uncontrollable urge to urinate.
Fecal Incontinence – Involuntary bowel or gas leakage.
Overactive Bladder Disorder (OAB) - Sometimes referred to as polyuria, overactive bladder disorder (OAB) refers to a condition in which urine is uncontrollably and unintentionally released from the bladder. Symptoms include a sudden and strong need to immediately urinate, as well as leakage occurring after the urge to urinate. Urinating 8+ times during the day or 2+ times at night can be indicators of OAB.
Pelvic Organ Prolapse – Prolapsing of the vagina, bladder, uterus, rectum, or small bowel. A prolapse is not always visible as it can cause descending inside or outside the vaginal canal or anus.
Dysuria – Pain when urinating. Can include a burning, tingling, or stinging feeling in the urethra or meatus.
Chronic Constipation - Defined as fewer than 3 bowel movements per week. Straining to pass stool or the sense of not emptying the bowel completely.
Dyspareunia (Painful Intercourse) - Can be caused by tight pelvic floor muscles, scarring on the perineum from childbirth (e.g. episiotomy, forcept delivery, vaginal tears), dystrophy, trauma, and more.
Symphysis Pubis Dysfunction (Pelvic Girdle Pain) - Pain in the pelvic joints, lower back, hips, thighs, pubic bone, and/or perineum. Often experienced during pregnancy (1 and 4 pregnant women experience this condition) making it challenging to walk.
Episiotomy and Vaginal Tears - Episiotomy is an incision made during childbirth between the vaginal opening and the anus to help facilitate birth. Vaginal tearing of the perineum are common in childbirth at varying degrees. Both these conditions cause scarring which can cause painful intercourse. Perineal massage performed by a physiotherapist can help relieve the discomfort.
Other Dysfunctions or symptoms where Pelvic Physiotherapy can help as part of the treatment plan
Pelvic Congestion Syndrome - A vascular disorder where the veins in the pelvic region are not able to properly drain blood. It causes chronic pelvic pain making intercourse, standing, and physical activity uncomfortable. It can also lead to hemorrhoids, lower back pain, varicose veins, and swelling of. the vulva.
Interstitial Cystitis (Bladder Pain Syndrome) - A chronic health issue that can sometimes feel like a bladder infection and can cause pain when having sex. The pain (and pressure) arises as the bladder begins to fill and it causes urinary frequency/incontinence or urgency. For women the pain is in the vulva or vagina and for men it can be felt in the scrotum, testicle, or penis.
Dysmenorrhea - Severe menstrual cramps and pain during ones period.
Prostatitis and Enlarged Prostate- Condition where the prostate becomes swollen, tender, and inflamed which can lead to conditions treatable with physiotherapy including urinary urge, painful urinration, lower back pain, painful ejaculation. Enlarged prostate is just as it sounds and happens with aging. It can cause urge incontinence and frequent urination.
Chronic Pelvic Pain - This can feel like pain and pressure in any of the pelvic organs including the bladder, rectum, uterus, vagina, urethra. Can be caused by other pelvic dysfunctions or weakened pelvic floor muscles. However at times this can be caused by a serious condition that requires further investigation by your healthcare provider including Endometriosis, ectopic pregnancy, Urinary Tract Infection, Pelvic Inflammatory Disease, Pelvic Congestion Syndrome, Irritable Bowel Syndrome, Uterine Fibroids, Levator Syndrome,
Pudendal Neuralgia - Pain, discomfort, or numbness in the pelvic or genitals that happens with the large nerve (pudendal nerve) that runs from the back of the pelvis to the genitals becomes irritated.
Want a Free Pelvic Consultation?
Quality Care Practitioners are offering free pelvic consultations before you book an assessment.
How Pelvic Floor Physiotherapy Can Help
Pelvic floor physiotherapy (PFPT) can be beneficial for treating any type of pelvic floor dysfunction, which typically occurs when your muscles are either too weak, or too tight. PFPT begins with an assessment of your symptoms and condition, which involves an external and internal examination of the pelvic floor muscles in order to identify a course of treatment. PFPT is tailored to your individual needs, and will therefore look different depending upon your specific condition. Treatments can range from exercises and manual treatments to electronic monitoring in order to train your muscles back into effective working condition. Pelvic floor physiotherapists can offer advice about daily activities, including proper bladder and bowel habits.
Kegels and How to Exercise Your Pelvic Floor
Kegels refer to a set of exercises which can help strengthen your pelvic floor muscles in order to tighten and contract those muscles which support your bladder, uterus, small intestine, and rectum. Kegel exercises can benefit you if you experience leakage when sneezing, laughing, or coughing; have a strong and sudden urge to urinate; or leak stool. One type of kegel exercise begins with trying to urinate-- once you begin to urinate, squeeze your muscles in order to cease urination. At this stage, you should feel your muscles lift-- this is a kegel. Repeat this process as you urinate, though it is not recommended that you do kegels every time you pee, as this can cause problems such as urinary tract infections.
Kegels can also be done when you are not urinating-- simply squeeze your pelvic floor muscles for 3 seconds, release for 3 seconds, and repeat this process 10 times in order to complete 1 set of kegels.
Kegels are not the only type of exercise for strengthening your pelvic floor muscles.
Other exercises include knee folds, toe taps, and hip bridges. Knee folds begin by lying on your back with your knees bent. Slowly lower one knee to the floor, and proceed to bring that knee back up. Repeat this process with both knees. Toe taps also begin on your back, and involve lifting your legs up to a tabletop surface, and back down to the floor. Hip bridges involve bringing your hipbones upwards to the sky, and slowly lowering back down to the floor (beginning with your upper back, followed by middle, and lower back) and releasing your pelvic floor muscles once your back has fully reached the floor.
Why To See a Pelvic Health Practitioner
It is often much harder than you think to perform a proper kegel or to isolate certain areas of the pelvic floor and peripheral muscle groups to do the exercises that are best for your situation. A Pelvic practitioner like a Pelvic Floor Physiotherapist can perform a full assessment (including an internal exam if you choose) and help coach you through the proper breathwork, contractions, positioning, and more. They can also give visual cues, help you find the sensation (especially if there is scar tissue or nerve damage from childbirth). They can also give you tips such as hip or quad strengthening exercises that can improve your pelvic strength as well. Sometimes they also help with stretching of the vaginal muscles or perform a perineum massage to reduce scar tissue damage and discomfort. It is a complex area of the body and unlike fitness classes that are one-size-fits all, pelvic floor exercise programs are highly personal based on the individuals condition. To see a Quality Care pelvic floor health expert book an assessment here or if not ready, you can request a free discovery call.
Virtual Pelvic Support On-Demand
Want to submit a question and get a personalized video answer back? We have partnered with Wellby where you can ask their Pelvic specialists questions online and skip the appointment altogether. It’s free to join and their women’s health experts are curated from around the world and seen in publications including Cosmopolitan, Women’s Health Magazine, Elle, and more.